Why CPT Codes Are Where Billing Breaks or Works
If you have ever wondered why clean claims still get denied or why reimbursements do not match the care you provided, CPT codes are often the reason. These codes sit at the center of medical billing accuracy, yet they are one of the most misunderstood parts of the revenue cycle.
Here’s the thing. CPT coding is not just about picking the closest code and moving on. Small mistakes compound quickly. They trigger denials, audits, delayed payments, and frustrated staff.
If you run a medical practice in the United States and deal with insurance billing, you are not alone. This guide walks you through what CPT codes are, why they matter, and how to implement them correctly so your claims get paid the first time.
What We’ll Cover
- What CPT codes are and how they work
- Why CPT coding accuracy directly affects revenue
- Common CPT code errors that lead to denials
- CPT coding guidelines and best practices
- How to implement a repeatable CPT coding process
What CPT Codes Are and How They Actually Work
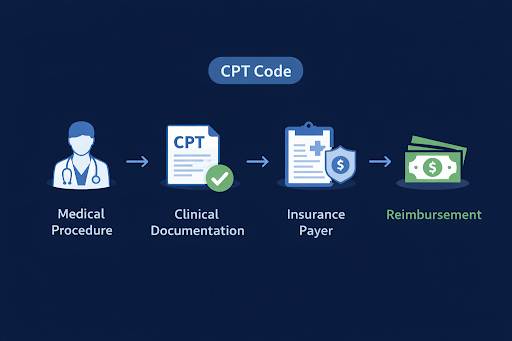
CPT codes, short for Current Procedural Terminology codes, describe the medical services and procedures you provide. They tell payers exactly what was done, how it was done, and in many cases, how complex it was.
Each CPT code is tied to:
- A specific service or procedure
- Documentation requirements
- Payer-specific reimbursement rules
What this really means is that CPT codes are not just labels. They are instructions. If the code does not match the documentation or payer rules, the claim fails.
CPT codes fall into three main categories:
- Category I: Common procedures and services
- Category II: Performance tracking and quality measures
- Category III: Temporary and emerging technologies
Most billing errors happen in Category I coding, where complexity and volume are highest. For a deeper foundation, it helps to understand what medical coding is and why it is essential for healthcare practices.
Why CPT Coding Accuracy Directly Impacts Revenue
CPT coding errors are one of the top causes of claim denials across all specialties. Even when the clinical care is perfect, incorrect coding creates revenue leakage.

Accurate CPT coding affects:
- Claim approval rates
- Reimbursement amounts
- Audit risk
- Compliance standing
Here’s a simple example. Undercoding leaves money on the table. Overcoding raises red flags and increases audit risk. Both outcomes hurt cash flow.
Practices that follow CPT coding guidelines consistently see:
- Faster claims processing
- Fewer payer rejections
- More predictable revenue
Coding accuracy is not about maximizing codes. It is about matching the service, the documentation, and the payer rule every time. This connection between coding and collections is a core pillar of effective revenue cycle management services.
Common CPT Code Errors That Lead to Denials

Most CPT errors are preventable. They usually come from rushed workflows, outdated knowledge, or unclear documentation.
The most common CPT coding mistakes include:
- Using outdated or deleted CPT codes
- Missing required modifiers
- Mismatched diagnosis and procedure codes
- Insufficient documentation for code level
- Unbundling services incorrectly
One of the biggest issues is documentation mismatch. The provider performs the service, but the note does not support the code billed. Payers do not assume intent. They only review what is documented.
Another frequent issue is modifier misuse. Modifiers are powerful but risky. Incorrect modifier use almost guarantees payer scrutiny. Many of these issues overlap with the broader causes outlined in medical billing denials and how to prevent them.
CPT Coding Guidelines Every Practice Should Follow

Here are medical coding best practices that consistently improve accuracy:
- Code from finalized documentation only
- Follow specialty-specific CPT guidelines
- Verify payer-specific CPT rules regularly
- Use modifiers only when fully supported
- Audit coding patterns quarterly
Let’s break this down. CPT rules change every year. What worked last year may not work now. Relying on memory instead of current guidelines creates silent errors that stack up over time.
Practices that build CPT updates into their workflow avoid surprises and maintain clean claims. Many practices formalize this process through dedicated medical coding services.
How to Implement CPT Codes Correctly in Daily Billing
Understanding CPT codes is only half the job. Implementation is where most practices struggle.

A reliable CPT coding workflow includes:
- Clear clinical documentation standards
- Trained coding review before claim submission
- Technology that flags errors early
- Regular internal or external audits
Documentation should always answer three questions:
- What service was provided
- Why it was medically necessary
- How complex the service was
Coding teams should never guess. If documentation is unclear, it must be clarified before billing. This step alone prevents a large percentage of denials.
Consistency matters. When every claim follows the same review process, accuracy improves and staff stress drops.
How Accurate CPT Coding Supports Faster Claims and Fewer Denials

Payers reward predictability. When your CPT coding aligns with guidelines and documentation, claims move faster.
Practices that implement structured CPT processes often experience:
- Fewer rework cycles
- Reduced accounts receivable days
- Lower denial rates
- Stronger payer trust
What this really means is fewer billing headaches and more time focused on patient care. These outcomes mirror the results seen in real-world revenue cycle management case studies.
Built on Real-World Coding Experience
At MedVoice, CPT coding is not handled in isolation. It is part of a full revenue cycle strategy built on accuracy, compliance, and speed.

With over 20 years in medical billing and coding, MedVoice supports practices across the United States with:
- 98 percent coding accuracy
- Less than 3 percent denial rates
- Faster claims processing
- Full HIPAA compliance
Our teams work alongside providers, not after the fact. Coding decisions are reviewed against real documentation and payer rules before claims go out the door.
That experience shows up in cleaner claims and more predictable revenue.
If your practice is dealing with frequent denials, inconsistent reimbursements, or coding confusion, it may be time to get help.
Here is the natural next step for many practices:
- Review your current CPT coding process
- Identify patterns in denials or underpayments
- Explore expert medical coding support
Ready to improve coding accuracy without overloading your staff? You can start by reviewing our approach to coding or reaching out through our contact page for a focused discussion.
Frequently Asked Questions About CPT Codes
What are CPT codes used for in medical billing?
CPT codes describe the medical services and procedures provided to patients. Insurers use them to determine reimbursement and claim approval.
How often do CPT codes change?
CPT codes are updated annually. New codes are added, some are revised, and others are deleted. Using outdated codes can lead to denials.
What is the difference between CPT codes and ICD codes?
CPT codes describe what service was performed. ICD codes explain why the service was medically necessary.
Can incorrect CPT coding trigger audits?
Yes. Overcoding, modifier misuse, and inconsistent patterns can increase audit risk and payer scrutiny.
Who should be responsible for CPT coding in a practice?
Coding should be handled by trained professionals who understand CPT guidelines, documentation standards, and payer rules.
How can I reduce CPT-related claim denials?
Clear documentation, updated coding knowledge, regular audits, and expert review significantly reduce CPT-related denials.
Accurate CPT Coding Leads to Predictable Revenue
CPT codes are not just a billing formality. They are the foundation of accurate reimbursement, compliance, and financial stability.
When CPT coding is done right, claims move faster, denials drop, and revenue becomes predictable. When it is rushed or inconsistent, small errors quietly drain your bottom line.
If you want to strengthen your billing process, reduce denials, and feel confident in your coding accuracy, learning and implementing CPT codes correctly is the place to start. You can explore more insights in the MedVoice blogs or take the next step by connecting with our team.