Your revenue cycle is supposed to be the heartbeat of your practice — yet for many providers, it feels more like a slow leak. You submit claims, wait weeks for payment, and still end up writing off thousands in unpaid balances.
The Pain Points We Hear Every Day:
- “Our A/R is getting out of control.”
- “We’re resubmitting the same denials again and again.”
- “Collections are down, but our billing costs keep going up.”

These aren’t just billing issues — they’re system issues. Poor eligibility checks, missing documentation, coding errors, and lack of denial follow-up create a domino effect that drains revenue and staff morale.
Why Generic RCM Services Fall Short
Many practices outsource RCM to cut costs, only to discover that “low-cost” billing actually means:
- Limited follow-up on denials
- Minimal reporting or insight into revenue trends
- No proactive approach to fixing systemic issues

MedVoice’s RCM Approach
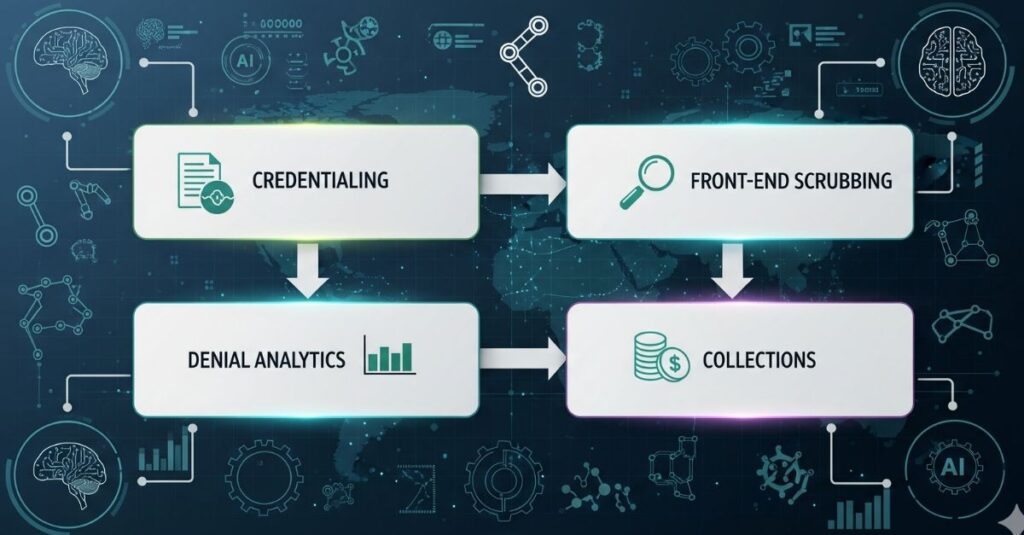
At MedVoice, we look at the entire revenue cycle, not just the billing step:
- Credentialing Checks: We verify provider enrollment before claims ever go out
- Front-End Scrubbing: AI-powered tools flag coding/documentation errors instantly
- Denial Analytics: We don’t just fix denials — we prevent them from happening again
Practices that work with MedVoice see a 15–20% boost in collections within 90 days, simply because revenue stops slipping through the cracks.

Takeaway: If your cash flow feels unpredictable, the problem might not be your payers — it might be your process.






