Understanding Medical Billing and Coding: Why It Matters to Every Practice
If your clinic’s revenue feels unpredictable, or you’re spending more time chasing claims than seeing patients, you’re not alone. Many healthcare providers struggle to understand where billing ends and coding begins, and how these two critical processes affect their cash flow.
In this guide, we’ll break down medical billing and coding in plain language, explain how they work together, and show how understanding the difference can protect your revenue and reduce denials.
Whether you manage a small practice or oversee multiple departments, you’ll walk away knowing exactly how to streamline both and what modern AI-driven tools can do to make the process faster, easier, and more accurate.
Quick Guide
- What’s the difference between billing and coding?
- Why they’re both critical to your revenue cycle
- Common challenges and errors that cost practices money
- How AI is changing medical billing and coding
- What to look for in a reliable RCM partner

Medical Coding: The Foundation of Every Claim
Medical coding is the translation step between patient care and payment. Each diagnosis, test, or treatment gets converted into standardized alphanumeric codes such as ICD-10, CPT, and HCPCS. These codes tell insurers what was done and why it was necessary.
Here’s the thing: coding isn’t just data entry. It requires precision and context. A single digit error or an outdated modifier can lead to claim denials or underpayment.es with 98% coding precision can see up to 30% faster collections and significantly lower denial rates.
Accurate coding ensures:
- Correct reimbursement for services rendered
- Compliance with payer rules and federal guidelines
- Reliable performance data for audits and reports
At MedVoice, we’ve seen how coding accuracy directly impacts revenue. Practices with 98% coding precision can see up to 30% faster collections and significantly lower denial rates.
In short, coding creates the financial language your billing system needs to communicate effectively with insurers.
If you’d like to explore deeper insights, check out Medical Coding: Ensuring Accuracy and Compliance in Healthcare Billing.
Medical Billing: Turning Codes into Cash
Once coding is complete, billing takes over. Medical billing is the process of submitting, tracking, and following up on claims to ensure healthcare providers get paid.
This involves:
- Preparing and submitting claims to insurance payers
- Managing rejections or denials
- Posting payments and reconciling accounts
- Sending patient statements when applicable
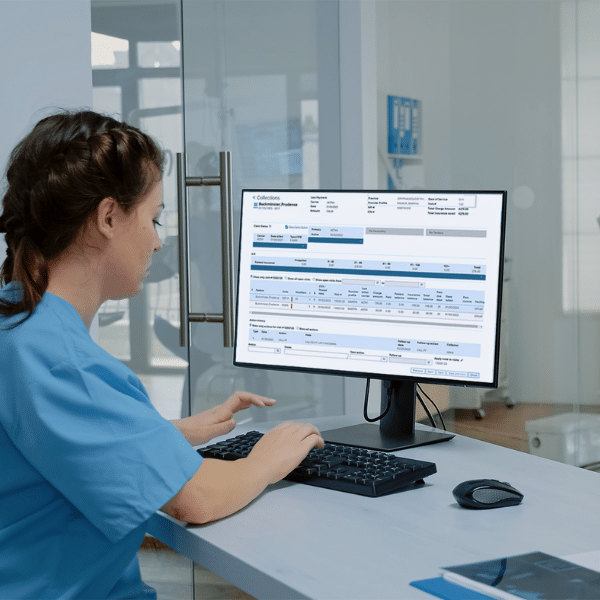
Where coding defines what was done, billing ensures payment for how much.
Even a well-coded claim can be delayed or denied if billing isn’t handled with precision. That’s why most successful practices treat billing as an ongoing, data-driven process rather than a back-office task.
With AI-powered systems such as those used by MedVoice, billing teams can detect missing fields, predict denial risk, and automate follow-ups while maintaining compliance and transparency.
You can learn more about our full process here: Revenue Cycle Management (RCM): Optimizing Healthcare Operations.
The Key Differences Between Medical Billing and Coding
Let’s make it simple.
| Aspect | Medical Coding | Medical Billing |
| Purpose | Translate care into standardized codes | Submit coded data for reimbursement |
| Primary Focus | Accuracy, compliance, and documentation | Payments, claims follow-up, and collections |
| Tools Used | ICD-10, CPT, HCPCS, EHR systems | Clearinghouses, claim scrubbing tools, RCM platforms |
| Required Skill | Clinical understanding, attention to detail | Financial management, payer knowledge |
| Outcome | Valid coded record | Successful reimbursement |
While these are distinct functions, they work best when integrated. Coding errors can create billing delays, and billing inefficiencies can hide coding mistakes. The most effective practices align both through a unified revenue cycle management service.

Why Both Matter: The Revenue Cycle Connection
Every dollar in your practice passes through the same route: the revenue cycle. Coding and billing are two halves of that system.
Here’s how they connect:
- A patient visit is documented by clinicians.
- Medical coders translate the documentation into precise codes.
- Billers submit claims based on those codes to insurers.
- Payers review and reimburse approved claims.
- Denied claims return for review, correction, and resubmission.
When either step fails, money stalls.
That’s why more practices are investing in AI-integrated RCM systems that merge billing and coding functions. These systems reduce redundancy, flag potential denials, and use predictive analytics to improve turnaround times.
The result is higher revenue, fewer headaches, and happier teams.You can also explore our related article: 5 Ways RCM Services Can Improve Your Cash Flow.
Common Mistakes That Hurt Revenue
Even experienced practices lose money from small, avoidable errors. Some of the most common include:
- Inaccurate coding: Missing modifiers or mismatched diagnosis codes.
- Late claim submission: Caused by workflow delays or incomplete documentation.
- Denied claims not followed up: Up to 65% of denied claims are never resubmitted.
- Poor documentation: Missing notes that justify procedures.
- Lack of communication: Between coders, billers, and providers.
AI-driven platforms such as those developed by MedVoice catch these issues automatically, ensuring no claim falls through the cracks.For better documentation practices, read Why Choose MedVoice for Comprehensive Healthcare Documentation Services.
How AI is Transforming Billing and Coding
Artificial Intelligence isn’t replacing people; it’s removing friction.
Modern RCM tools powered by AI help healthcare teams:
- Detect coding inconsistencies in real time
- Automate charge capture and data entry
- Predict which claims are likely to be denied
- Generate compliant documentation faster
- Reduce turnaround time for A/R collections
At MedVoice, our systems combine over 20 years of healthcare expertise with intelligent automation to deliver measurable outcomes including 98% coding accuracy, 40% faster claim turnaround, and fewer denials.
What this really means is that you can stop worrying about paperwork and start focusing on patient care again.
Discover more on The Evolution of Revenue Cycle Management: Adapting to Modern Healthcare Needs.
EEAT in Action: Experience, Expertise, Authority, Trust
Trust in medical RCM doesn’t come from marketing; it comes from results.
For two decades, MedVoice has supported healthcare providers across the United States with secure, HIPAA-compliant billing and coding solutions. Our team includes certified coders, experienced billers, and data specialists who understand both payer rules and clinical workflows.
When you read about 98% accuracy and faster collections, those aren’t inflated claims. They’re client-verified outcomes backed by continuous training and QA processes.
That’s what real expertise looks like. You can explore one of our success stories here: Case Study: Revenue Cycle Management.
Ready to Simplify Your Billing and Coding?
If you’ve ever wondered how much time your team spends fixing denials or tracking missing claims, it’s time to find out.
MedVoice helps clinics, hospitals, and specialty practices streamline their entire revenue cycle with AI-enhanced billing and coding that simply works.
Ready to take the next step? Explore Our RCM Services or Schedule a Consultation to see how simple accuracy can be.
Frequently Asked Questions
What is medical coding used for?
Medical coding translates every diagnosis, treatment, and service a healthcare provider delivers into universal alphanumeric codes that insurance companies, hospitals, and government programs understand. These codes such as ICD-10, CPT, and HCPCS, serve three major purposes:
- Reimbursement: They ensure the provider is paid accurately for each service performed.
- Compliance: They maintain legal and regulatory accuracy in patient records.
- Analytics: They allow healthcare systems to analyze performance, patient outcomes, and costs.
Without accurate coding, insurance claims can be delayed or denied, which directly impacts cash flow. Coding also supports audits and helps identify trends in patient care.
Learn more in our detailed guide: Medical Coding Services.
How is medical billing different from coding?
Medical coding lays the groundwork for billing. Coders identify what was done, and billers ensure those actions are paid for.
Coding focuses on assigning the correct diagnostic and procedural codes, while billing focuses on claim creation, submission, and payment tracking.
Here’s the simplest way to think of it:
- Coders translate care into codes.
- Billers translate codes into claims and payments.
Both are essential. Without accurate coding, claims are wrong. Without effective billing, even perfect claims go unpaid.
You can explore more about the billing process in Medical Billing Services.
Do I need both a biller and a coder in my practice?
Yes, because they handle different stages of the revenue cycle. Coders ensure the medical record is correctly translated into billing data, while billers ensure that data turns into cash flow.
In smaller practices, one person may perform both roles, but this can become risky as complexity increases. Many providers outsource to specialized RCM firms such as MedVoice, which combine certified coders and billing experts within the same workflow, supported by AI tools.
The benefit is faster collections, fewer denials, and a single team accountable for your revenue performance.
Learn about how integrated services work in Credentialing Services.
How can AI improve billing and coding accuracy?
AI improves billing and coding accuracy by automating repetitive tasks and identifying errors before they cause financial damage. For example:
- Real-time validation: AI cross-checks diagnosis and procedure codes for compliance.
- Predictive analysis: It flags claims likely to be denied and suggests corrections.
- Smart documentation: AI-powered transcription tools capture notes with clinical accuracy.
- Learning systems: Algorithms adapt to payer trends and detect evolving denial patterns.
At MedVoice, AI isn’t just a buzzword. It’s embedded into every step of our RCM process. It helps our experts focus on judgment calls while automation handles the routine work.
Read more about Medical Scribing: Transforming Physician Documentation and Patient Care.
What happens if my claims are denied?
Denied claims don’t have to mean lost revenue. When a claim is denied, the first step is root-cause analysis to understand why it failed. Common reasons include missing codes, mismatched data, or late submissions.
At MedVoice, our denial management process involves:
- Identifying the cause of denial
- Correcting the error quickly
- Resubmitting the claim with supporting documentation
- Tracking recurring issues to prevent future denials
The faster this process happens, the healthier your revenue cycle stays. With automation and experienced teams, we reduce denial turnaround times significantly and keep your collections consistent.
Check out our Medical Record Review for more on how review services support accuracy and compliance.
Is outsourcing billing and coding secure?
Yes, when handled by a HIPAA-compliant partner with the right systems in place. At MedVoice, data security is central to everything we do.
We use encrypted channels, strict access controls, and regular security audits. Every team member is trained in HIPAA and data protection standards. Our cloud-based platforms ensure sensitive patient data never leaves secure environments.
The result is complete transparency and compliance combined with the benefits of speed, accuracy, and cost efficiency.
Transform Your Revenue with Smarter Billing and Coding
Understanding the difference between billing and coding isn’t just academic. It’s the key to unlocking steady, predictable revenue.
By aligning both through a unified, AI-powered RCM solution, you reduce administrative drag, improve accuracy, and get paid faster.
If you’re ready to see how it works in real life, start here: MedVoice Revenue Cycle Management Services.