The healthcare revenue cycle is often seen as a necessary headache—a maze of codes, paperwork, and frustrating denials. But what if that complex cycle could be streamlined, accelerated, and nearly error-free?
That’s not a distant vision of the future — it’s the present reality with Revenue Cycle Management (RCM) Automation.
And at MedVoice, we’re not just predicting the future — we’re building it.
The True Cost of Manual Revenue Cycle Management
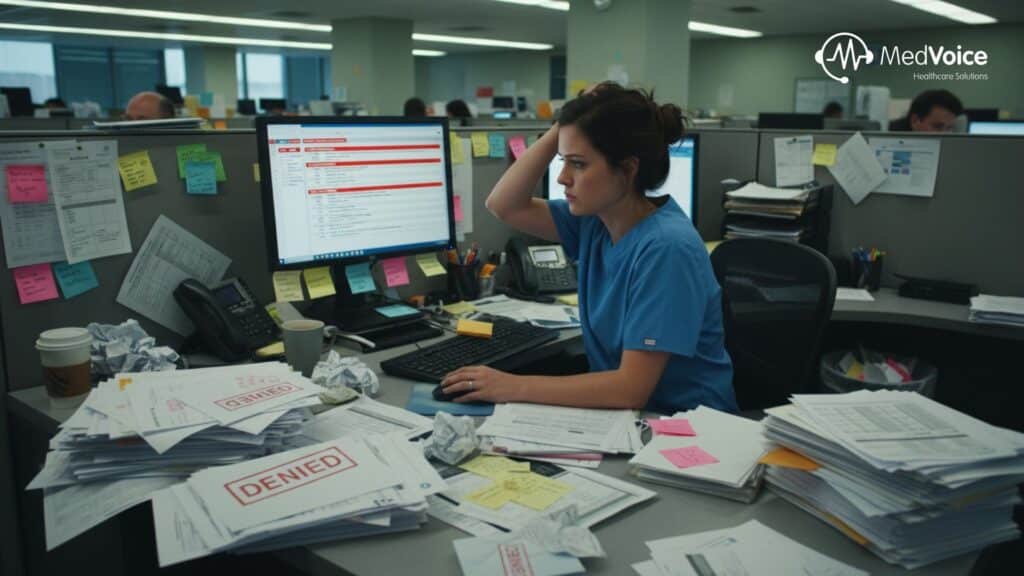
Healthcare providers today face immense pressure to deliver exceptional patient care while managing an increasingly complex financial ecosystem. Unfortunately, traditional, manual RCM processes remain the root cause of many inefficiencies and financial losses.
Here’s what manual RCM really costs healthcare organizations:
1. High Denial Rates
Minor data entry or coding errors can trigger claim denials, forcing costly and time-consuming appeals that delay reimbursements.
2. Slow Cash Flow
From patient intake to final payment posting, manual processes can drag the revenue cycle out for weeks or even months — creating cash flow strain.
3. Administrative Burden
Staff spend endless hours on repetitive tasks such as checking eligibility, posting payments, and managing follow-ups. This workload leads to burnout and diverts focus from patient care.
4. Compliance Risks
Keeping up with evolving payer rules and government regulations is a full-time job — and one mistake can result in fines or compliance penalties.
The MedVoice Solution: Automation that Pays for Itself

At MedVoice, we’re redefining the healthcare revenue cycle with intelligent automation that replaces inefficiency with accuracy, speed, and control.
Our RCM automation solutions transform your cycle from a slow, reactive process into a fast, proactive revenue engine.
Here’s how automation works — and why it’s a game changer.
1. Zero-Error Patient Intake & Eligibility Verification
Errors at the intake stage lead to costly denials later. MedVoice automation bots instantly verify a patient’s insurance eligibility and benefits across hundreds of payer portals — in real time.
Result: Potential issues are flagged before service is delivered, dramatically reducing downstream denials.
2. AI-Powered Claims Scrubbing & Submission
Our intelligent automation system reviews every claim to identify missing modifiers, code mismatches, or non-compliant data before submission.
Result: Higher clean claim rates, fewer denials, and faster reimbursements — directly boosting your cash flow.
3. Proactive Denial and Follow-Up Management
When claims are denied or underpaid, MedVoice automation identifies, categorizes, and prioritizes them automatically. The system even initiates follow-ups — drafting appeal letters or checking claim statuses — without manual intervention.
Result: Improved revenue recovery and significantly lower Days Sales Outstanding (DSO).
Why Choose MedVoice for RCM Automation?
| Benefit | What MedVoice Automation Delivers | Why It Matters |
| Increased Revenue | Higher clean claim rates and faster denial resolution. | Boosts your bottom line and minimizes write-offs. |
| Reduced Errors | Rule-based systems for verification and coding. | Mitigates compliance risks and reduces rework. |
| Lower Costs | 24/7 digital workforce managing repetitive tasks. | Frees up staff for strategic or patient-focused work. |
| Enhanced Patient Experience | Faster, more transparent billing with fewer surprises. | Increases patient trust and retention. |
🎯 Automation: The Only Sustainable Path Forward
The healthcare industry is evolving rapidly — and so are its administrative challenges. Relying solely on manual RCM processes is no longer sustainable for organizations aiming to stay financially strong and compliant.
Automation is the undeniable future of Revenue Cycle Management.
With MedVoice, you gain the efficiency, accuracy, and compliance your organization needs to stay ahead in today’s healthcare environment.
Stop managing your cycle manually. Start automating your success with MedVoice.
Ready to Automate Your Revenue Cycle?
Don’t let manual errors and delays impact your revenue. Discover how MedVoice’s intelligent RCM automation can reduce denials, accelerate cash flow, and elevate operational efficiency.
📞 Contact us today for a personalized RCM Automation Assessment!
📧 Sales@medvoiceinc.com
🌐 www.medvoiceinc.com
📱 +1 469-402-3160
Follow MedVoice RCM Insights
Stay informed about the latest trends in RCM automation and healthcare technology.
📬 Subscribe on LinkedIn: MedVoice Newsletter








