The Real Reason Your Practice Is Losing Revenue
Every healthcare practice faces the same silent threat: delayed payments, denied claims, and documentation errors that quietly eat away at cash flow. If you’re a clinic owner, physician, or billing manager trying to figure out why your revenue isn’t matching your patient load, you’re not alone.
Here’s the thing: most practices don’t lose money because of bad medicine. They lose it because of broken billing systems.
This guide explains what revenue cycle management (RCM) really means, why it matters more than ever, and how to fix it using smarter tools and processes.
By the end, you’ll know exactly how to improve your collections, reduce denials, and get paid faster with insights from over 20 years of MedVoice experience helping healthcare organizations across the U.S. do just that.
What We’ll Cover
- What Revenue Cycle Management Actually Is
- The 7 Key Stages of the Healthcare RCM Process
- Common Revenue Leaks (and How to Stop Them)
- How AI and Automation Are Transforming RCM
- Real-World Results: How Practices Are Improving Collections
- FAQs About RCM and Billing Optimization
- How to Take the Next Step Toward Better Revenue Flow
What Is Revenue Cycle Management (RCM)?
Revenue Cycle Management is the process that tracks every dollar a healthcare organization earns, from the moment a patient books an appointment to when the final payment is posted.
In simple terms, it’s your financial heartbeat. If it works well, your practice runs smoothly. If it doesn’t, you’ll feel it everywhere—in cash flow, patient satisfaction, and team stress.
RCM covers these core steps:
- Patient registration and insurance verification
- Service documentation and medical coding
- Claim submission
- Payment posting
- Denial management
- A/R follow-up
Reporting and optimization
Each step depends on accuracy, timing, and compliance. Miss one detail—a code, a modifier, or a payer rule—and your reimbursement slows to a crawl.

Why RCM Matters More Than Ever
Healthcare has become more complex. Payer rules change constantly, staffing shortages create bottlenecks, and manual billing errors can cost clinics thousands every month.
Your ability to collect revenue efficiently now depends on how well your RCM system performs.
When RCM is optimized, practices see:
- Faster collections: Claims get paid in weeks, not months.
- Fewer denials: AI coding accuracy can reach up to 98%.
- Better compliance: HIPAA standards are automatically enforced.
- Lower admin costs: Staff spend less time chasing claims.
When RCM is neglected, revenue leaks start small but eventually snowball.
The 7 Stages of the RCM Process (and Where Money Slips Away)
Let’s break it down.
Patient Registration and Verification
If insurance details aren’t verified upfront, denials are almost guaranteed later.
Best practice: Automate eligibility checks before every visit.
Charge Capture and Coding
Coding errors are the number one reason for denied claims.
Best practice: Use AI-assisted coding tools that flag mismatches and improve accuracy.
Claim Submission
Timing is everything. Submitting claims late leads to delayed payments.
Best practice: Batch and submit claims daily, not weekly.
Payment Posting
Accurate posting helps you spot payer trends and underpayments early.
Best practice: Reconcile payments against contracts automatically.

Denial Management
Every denied claim is lost revenue unless appealed.
Best practice: Track denial reasons and build rules to prevent repeats.
Accounts Receivable Follow-Up
Old A/R balances are red flags.
Best practice: Automate follow-ups and prioritize high-value claims.
Reporting and Continuous Improvement
What you don’t measure, you can’t fix.
Best practice: Review key metrics monthly—clean claim rate, A/R days, and denial rate.
At MedVoice, we’ve seen clinics recover up to 30% more revenue simply by improving processes in steps two through six.
The Biggest RCM Challenges (and How to Fix Them)
Even the best practices struggle with:
- Rising denial rates due to payer changes
- Staff shortages that cause bottlenecks
- Inconsistent documentation between clinical and billing teams
- Inefficient follow-ups on unpaid claims
In most cases, 10–20% of revenue is lost every month without anyone realizing it.
The fix is a combination of human expertise and smart automation.
AI tools can flag errors, auto-code common cases, and handle repetitive tasks. Skilled billing teams then focus on complex or high-value claims.
That’s the balance MedVoice brings: technology that works fast and people who understand healthcare.
Learn more about 5 ways RCM services can improve your cash flow.
How AI Is Changing the Future of RCM

Artificial intelligence isn’t replacing billing teams. It’s empowering them.
Here’s how:
- Voice-to-text documentation: Converts provider notes into coded documentation in seconds.
- AI-powered coding: Detects missing or incorrect CPT/ICD codes instantly.
- Predictive analytics: Identifies claim risk before submission.
- Automated denial management: Learns from payer behavior to prevent future denials.
The result is a 40% faster A/R turnaround and up to 98% coding accuracy—benchmarks achieved by practices using MedVoice’s AI RCM suite.
Real Results: What Optimized RCM Looks Like
A family clinic in Texas was struggling with slow collections and constant denials. Within 90 days of switching to MedVoice, they:
- Reduced A/R days from 62 to 34
- Increased collections by 28%
- Cut manual billing hours in half
See how in this RCM case study.
That’s the impact of accurate coding, proactive follow-ups, and intelligent automation working together.
It’s not about replacing your billing team. It’s about making them unstoppable.

Why Choose MedVoice

If your current RCM process feels more like a guessing game than a growth engine, it’s time for a smarter approach.
At MedVoice, we’ve spent over two decades refining every step of the revenue cycle. From credentialing to claim submission, our systems are built to deliver measurable results: faster payments, fewer denials, and cleaner claims.
Our team partners directly with clinics, hospitals, and medical centers across the U.S., helping them regain control over cash flow without overhauling their entire operation.
You’ll see transparency, accountability, and real-time reporting that keeps your revenue predictable and your team focused on patients, not paperwork.Explore why practices choose MedVoice for comprehensive documentation services.
Ready to Improve Your Collections?
Let’s make your billing work for you.
Schedule a Consultation with MedVoice to review your current RCM process.
We’ll show you exactly where revenue is leaking and how to fix it using AI-backed solutions that align with your workflow rather than disrupt it.
Frequently Asked Questions About RCM
What does revenue cycle management include?
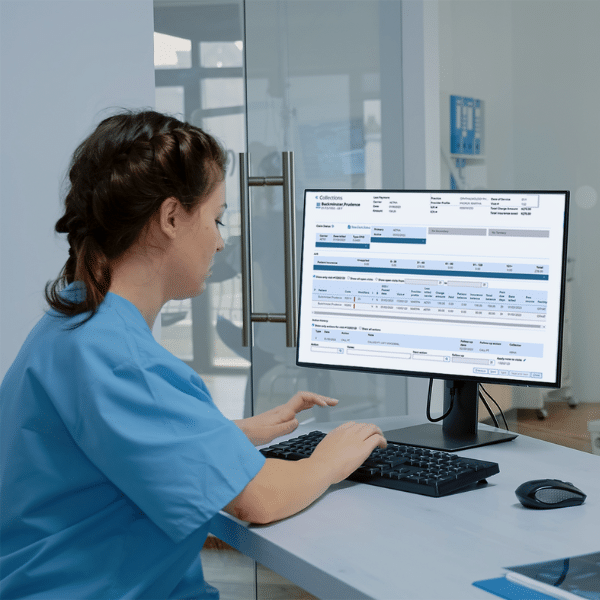
Revenue Cycle Management covers every administrative and financial touchpoint between the patient and the provider. It begins with patient registration and insurance verification, followed by charge capture, medical coding, claim submission, payment posting, and denial management. The cycle closes with reporting and performance optimization.
Each step affects how quickly and accurately a practice gets paid. When managed properly, RCM eliminates revenue gaps, reduces claim rejections, and provides a clear view of financial health.
How can AI help with medical billing and coding?
AI can instantly identify coding errors, missing modifiers, or mismatched diagnosis codes before claims ever reach a payer. It also learns from payer behavior over time, predicting which claims are most likely to be denied and why.
AI-driven medical coding software from MedVoice helps translate clinical documentation into accurate CPT and ICD-10 codes in seconds, freeing providers from hours of manual entry. Learn more about streamlining medical billing for efficient operations.
How long does it take to improve cash flow with RCM optimization?
Practices typically start seeing measurable results within 60 to 90 days. In that time, automation tools begin reducing manual errors and flagging process inefficiencies.
When MedVoice conducts a full RCM audit, we focus on three fast-impact areas: coding accuracy, denial recovery, and A/R cleanup. These early wins often increase collections by 20–30% within the first quarter.
Is outsourcing RCM safe and HIPAA-compliant?
Absolutely. A reputable RCM partner must follow strict HIPAA and HITECH guidelines to protect patient data. At MedVoice, all systems are U.S.-based, encrypted end-to-end, and managed by certified billing professionals.
Outsourcing doesn’t mean losing control. It means gaining expertise. You’ll still have full visibility into reports, claim statuses, and payments through a secure dashboard while our team handles the heavy lifting.
What’s the ROI of outsourcing RCM?
The ROI varies by practice size, but most see:
- 25–40% faster collections
- 20–30% fewer claim denials
- Up to 50% reduction in billing staff hours
The long-term impact is even more valuable: predictable cash flow, cleaner financials, and less administrative burnout. Outsourcing RCM often pays for itself within the first few months through recovered revenue and efficiency gains.
Can small practices benefit from RCM services?
Yes. Small practices often benefit the most. They tend to have smaller admin teams juggling multiple roles, which increases the risk of coding errors and delayed billing.
With MedVoice’s AI-driven RCM system, small clinics can compete with larger organizations by automating billing, coding, and follow-ups without needing to expand staff. This helps independent physicians stay profitable while focusing more on clinical documentation.
Take Control of Your Revenue Flow
RCM isn’t just about billing. It’s about reclaiming the time, confidence, and predictability your practice needs to grow.
When done right, revenue cycle management turns from a back-office burden into a profit engine. With MedVoice’s AI-powered billing, coding, and documentation tools, you’ll collect faster, reduce denials, and eliminate the guesswork in your financial process.
Ready to see what optimized revenue looks like? Schedule a Consultation

Related Reads: